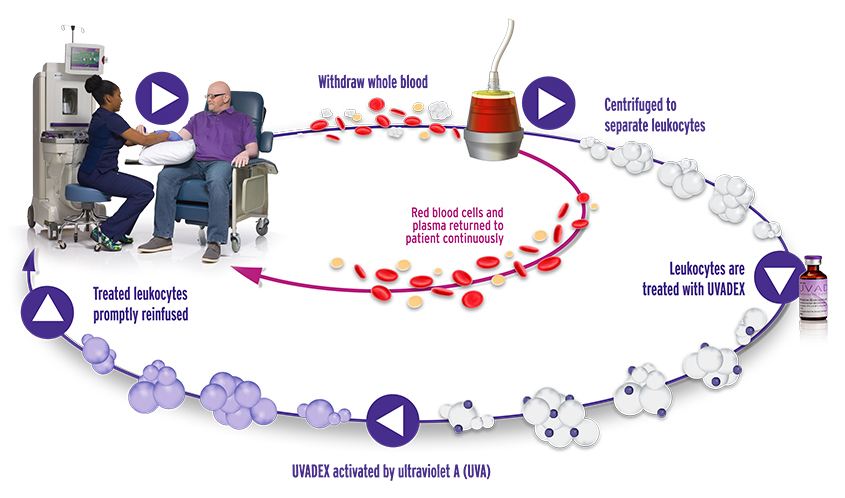
THERAKOS® Photopheresis Procedure1,2
Harness the immune system in managing skin manifestations of CTCL
-
Addressing the immune system imbalance may target the underlying cause of skin symptoms2-5*
*The exact mechanism of action of UVADEX is not known.
For illustrative purposes only.
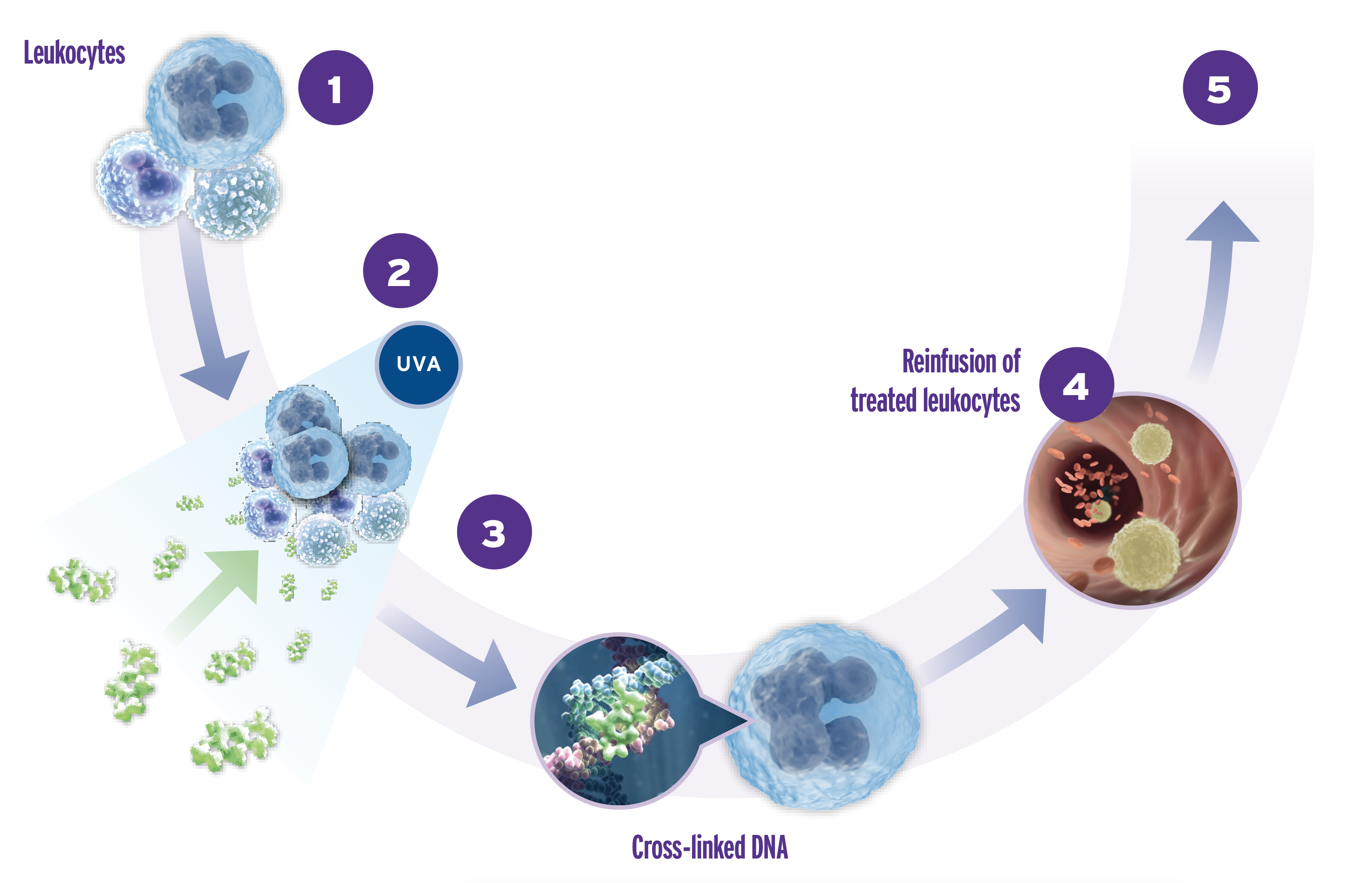
Potential Mechanism of Action*
Immunomodulation with THERAKOS Photopheresis
-
Blood is fractionated via centrifugation. The “buffy coat” (the fraction containing the majority of
leukocytes and platelets) is isolated and the remaining blood returned to the patient1 -
The buffy coat is treated with methoxsalen and then exposed to UVA light1
-
UVA activation of methoxsalen triggers cell death2,3,6-9
-
The buffy coat, containing living, dead, or dying cells; subcellular fragments; and soluble factors,
is released back into the patient’s bloodstream2,9-13 -
The treated leukocytes are engulfed by phagocytic cells, leading to a range of indirect
downstream immunomodulatory effects7,8,11,14,15
*The exact mechanism of action of UVADEX is not known.
-
While the exact mechanism of action continues to be investigated, THERAKOS® Photopheresis exhibits anticlonal cytotoxic characteristics in the treatment of CTCL skin manifestations and enhances the immunologic response to skin manifestations of the disease16,17
-
THERAKOS Photopheresis may induce an immunomodulatory effect against CTCL skin manifestations
-
ECP inhibits DNA synthesis and cell division, inducing cell death in treated leukocytes, including CTCL cells2-4
-
References:
-
THERAKOS® CELLEX® Photopheresis System Operator’s Manual. 1470493_Rev06_EN-US. Mallinckrodt; 2019.
-
UVADEX (methoxsalen) Sterile Solution (prescribing information). Therakos Inc; March 2021.
-
Yoo EK, Rook AH, Elenitsas R, Gasparro FP, Vowels BR. Apoptosis induction by ultraviolet light A and photochemotherapy in cutaneous T-cell lymphoma: relevance to mechanism of therapeutic action. J Invest Dermatol. 1996;107(2):235-242.
-
Gerber A, Bohne M, Rasch J, Struy H, Ansorge S, GolInick H. Investigation of annexin V binding to lymphocytes after extracorporeaI photoimmunotherapy as an early marker of apoptosis. Dermatology. 2000;201(2):111-117.
-
Hwang ST, Janik JE, Jaffe ES, Wilson WH. Mycosis fungoides and Sézary syndrome. Lancet. 2008;371(9616):945-957.
-
Caffieri S, Di Lisa F, Bolesani F, et al. The mitochondrial effects of novel apoptogenic molecules generated by psoralen photolysis as a crucial mechanism in PUVA therapy. Blood. 2007;109(11):4988-4994.
-
Knobler R, Berlin G, Calzavara-Pinton P, et al. Guidelines on the use of extracorporeal photopheresis. J Eur Acad Dermatol Venereol. 2014;28(suppl 1):1-37.
-
Hart JW, Shiue LH, Shpall EJ, Alousi AM. Extracorporeal photopheresis in the treatment of graft-versus-host disease: evidence and opinion. Ther Adv Hematol. 2013;4:320-334.
-
Craciun LI, Stordeur P, Schandené L, et al. Increased production of interleukin-10 and interleukin-1 receptor antagonist after extracorporeal photochemotherapy in chronic graft-versus-host disease. Transplantation. 2002;74:995-1000.
-
Caruso S, Poon IKH. Apoptotic cell-derived extracellular vesicles: more than just debris. Front Immunol. 2018;9:1486.
-
Tatsuno K, Yamazaki T, Hanlon D, et al. Extracorporeal photochemotherapy induces bona fide immunogenic cell death. Cell Death Dis. 2019;10:578.
-
Medina CB, Ravichandran KS. Do not let death us do part: 'find-me' signals in communication between dying cells and the phagocytes. Cell Death Differ. 2016;23(6):979-989.
-
Bisaccia E, Vonderheid EC, Geskin L. Safety of a new, single, integrated, closed photopheresis system in patients with cutaneous T-cell lymphoma. Br J Dermatol. 2009;161(1):167-169.
-
Marshall SR. Technology insight: ECP for the treatment of GvHD—can we offer selective immune control without generalized immunosuppression? Nat Clin Pract Oncol. 2006;3(6):302-314.
-
Morelli AE, Larregina AT, Shufesky WJ, et al. Internalization of circulating apoptotic cells by splenic marginal zone dendritic cells: dependence on complement receptors and effect on cytokine production. Blood. 2003;101:611-620.
-
Vieyra-Garcia PA, Wolf P. Extracorporeal photopheresis a case of immunotherapy ahead of its time. Tranfus Med Hemother. 2020;47:226-234.
-
Shiue LH, Alousi AM, Wei C, Hosing CM, Duvic M, Ni X. Augmentation of blood dendritic cells by extracorporeal photopheresis in patients with leukemic cutaneous T-cell lymphoma and graft-versus-host disease. J Invest Dermatol. 2013;133(8):2098-2100.
INDICATIONS AND USAGE
UVADEX® (methoxsalen) Sterile Solution is indicated for extracorporeal administration with the THERAKOS® CELLEX® Photopheresis System in the palliative treatment of the skin manifestations of Cutaneous T-Cell Lymphoma (CTCL) that is unresponsive to other forms of treatment.
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
UVADEX is contraindicated in:
-
Patients exhibiting idiosyncratic or hypersensitivity reactions to methoxsalen, other psoralen compounds, or any of the excipients
-
Patients possessing a specific history of a light-sensitive disease state, including lupus erythematosus, porphyria cutanea tarda, erythropoietic protoporphyria, variegate porphyria, xeroderma pigmentosum, and albinism
-
Patients with aphakia because of significantly increased risk of retinal damage
-
Patients that have contraindications to the photopheresis procedure
WARNINGS AND PRECAUTIONS
-
Patients who are receiving concomitant therapy (either topically or systemically) with known photosensitizing agents such as anthralin, coal tar or coal tar derivatives, griseofulvin, phenothiazines, nalidixic acid, halogenated salicylanilides (bacteriostatic soaps), sulfonamides, tetracyclines, thiazides, and certain organic staining dyes such as methylene blue, toluidine blue, rose bengal, and methyl orange may be at greater risk for photosensitivity reactions with UVADEX
-
Oral administration of methoxsalen followed by cutaneous UVA exposure (PUVA therapy) is carcinogenic. Methoxsalen also causes DNA damage, interstrand cross-links and errors in DNA repair
-
Methoxsalen may cause fetal harm when given to a pregnant woman. Women of childbearing potential should be advised to avoid becoming pregnant. If UVADEX is used during pregnancy, or if the patient becomes pregnant while receiving UVADEX, the patient should be apprised of the potential hazard to the fetus
-
Severe photosensitivity can occur in patients treated with UVADEX. Advise patients to wear UVA absorbing, wrap-around sunglasses and cover exposed skin or use a sunblock (SPF 15 or higher), and avoid all exposure to sunlight for twenty-four (24) hours following photopheresis treatment
-
After methoxsalen administration, exposure to sunlight and/or ultraviolet radiation may result in "premature aging" of the skin
-
Since oral psoralens may increase the risk of skin cancers, monitor closely those patients who exhibit multiple basal cell carcinomas or who have a history of basal cell carcinomas
-
Serious burns from either UVA or sunlight (even through window glass) can result if the recommended dosage of methoxsalen is exceeded or precautions are not followed
-
Exposure to large doses of UVA light causes cataracts in animals. Oral methoxsalen exacerbates this toxicity
-
Safety in children has not been established
-
Thromboembolic events, such as pulmonary embolism and deep vein thrombosis, have been reported with UVADEX administration through photopheresis systems for treatment of patients with graft-versus-host disease, a disease for which UVADEX is not approved
ADVERSE REACTIONS
-
Side effects of photopheresis (UVADEX used with the THERAKOS Photopheresis Systems) were primarily related to hypotension secondary to changes in extracorporeal volume (>1%)
INDICATIONS
IMPORTANT SAFETY INFORMATION
CONTRAINDICATIONS
The THERAKOS CELLEX Photopheresis System is not designated, sold, or intended for use except as indicated.
Certain underlying medical conditions contraindicate THERAKOS Photopheresis, including patients:
-
who cannot tolerate extracorporeal volume loss during the leukocyte-enrichment phase
-
exhibiting idiosyncratic or hypersensitivity reactions to 8-methoxypsoralen/psoralen compounds
-
with coagulation disorders
-
who have had previous splenectomy
WARNINGS AND PRECAUTIONS
-
THERAKOS Photopheresis treatments should always be performed in locations where standard medical emergency equipment is available. Volume replacement fluids and/or volume expanders should be readily available throughout the procedure
-
Patients who may not be able to tolerate the fluid changes associated with extracorporeal photopheresis should be monitored carefully
-
Procedures, such as renal dialysis, which might cause significant fluid changes (and expose the patient to additional anticoagulation) should not be performed on the same day as extracorporeal photopheresis
-
Individual patients may require a heparin dosage that varies from the recommended dose to prevent post-treatment bleeding or clotting during a treatment
ADVERSE REACTIONS
-
Hypotension may occur during any treatment involving extracorporeal circulation. Closely monitor the patient during the entire treatment for hypotension
-
Transient pyretic reactions, 37.7-38.9°C (100-102°F), have been observed in some patients within six to eight hours of reinfusion of the photoactivated leukocyte-enriched blood. A temporary increase in erythroderma may accompany the pyretic reaction
-
Treatment frequency exceeding labeling recommendations may result in anemia
-
Venous access carries a small risk of infection and pain








